Everything you need to know about how it changes
There is nothing more frustrating then when we are asked if we are before or on our menstrual cycle everytime we have a mood change. Or when we feel blue without a specific reason, only to realise that we just got our periods. Accept it or not our brain changes from the menstrual cycle.
Elma Jashim, a recent college graduate eagerly anticipates the start of medical school in the fall. However, she also dreads the emotional ups and downs that accompanies her monthly menstrual cycle and the potential disruption it could cause to her demanding academic schedule.
“I usually experience a sort of emotional limbo a few days before my period starts,” explains Jashim. During this time, she becomes more sensitive to even minor emotional triggers, which can lead to heightened reactions, such as feeling on the verge of tears over small mistakes at work.
While the precise neurological mechanisms underlying these emotional changes remain unclear, research is shedding light on how sex hormones impact the brain. Previous studies in animals have demonstrated that estrogen, a key hormone in female reproductive health, can influence the volume of certain brain regions. However, it was uncertain whether similar effects occurred in the human brain.
Recent MRI scans of women’s brains have revealed significant structural changes linked to the fluctuation of sex hormones throughout the menstrual cycle. This 29-day hormonal dance, which prepares the reproductive system for potential pregnancy, appears to dynamically reshape brain regions involved in regulating emotions, memory, behavior, and information processing efficiency.
“It’s truly remarkable to witness how rapidly the adult brain can adapt,” states Julia Sacher, a psychiatrist and neuroscientist at the Max Planck Institute for Human Cognitive and Brain Sciences in Leipzig, Germany, who spearheaded one of these groundbreaking studies.
The fact that the brain undergoes changes throughout the menstrual cycle holds particular significance due to the frequency with which most women experience approximately 450 menstrual cycles over a span of 30-40 years, according to Catherine Woolley, a neurobiologist at Northwestern University in Evanston, Illinois.
Catherine Woolley highlights the strength of these studies, noting that they involve both brain imaging and hormone measurements conducted on the same individuals across specific phases of the menstrual cycle.
Emily Jacobs, a neuroscientist at the University of California, Santa Barbara, emphasizes the emerging understanding of how influential these hormones are in shaping not only the physical structure but also the functional organization of the brain.
The menstrual cycle typically spans 25 to 30 days and commences with the shedding of the uterine lining, known as the “period.” Initially, female sex hormone levels in the bloodstream are at their lowest, gradually surging over the ensuing weeks. Estrogen levels increase first, prompting uterine lining growth, followed by a decline to release an egg from the ovary, marking the cycle’s midpoint. Subsequently, progesterone and estrogen levels rise for approximately seven days, preparing the uterine lining for potential egg fertilization. If pregnancy does not transpire, both estrogen and progesterone levels decline, triggering menstrual bleeding.
While the menstrual cycle is characterized by fluctuations in hormone levels, additional hormones like testosterone and cortisol also undergo cyclic patterns, peaking before dawn and declining by evening—a rhythm observed in both genders.
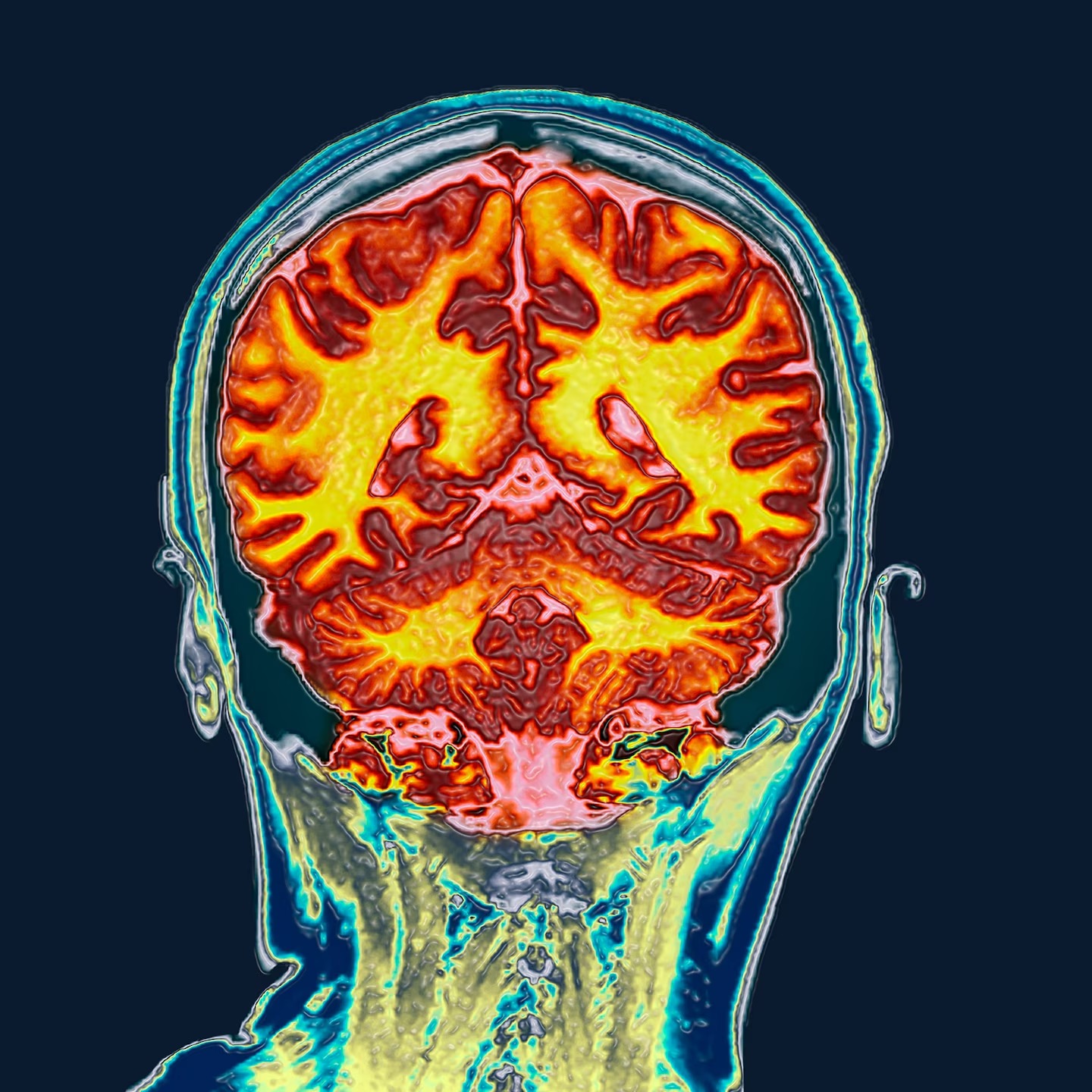
The brain consists of a dense network of cells known as neurons, resembling miniature trees. Within the outer layer of brain tissue, called gray matter, neurons and their short branches, known as dendrites, are found. These dendrites feature leaf-like protrusions called spines, while the roots, or axons, of neurons are densely packed within the brain’s white matter.
Gray matter plays a crucial role in regulating emotions, learning, and memory, while deeper within the brain tissue, white matter facilitates information exchange and connects various regions of gray matter.
The discovery that certain parts of the brain respond to female sex hormones dates back nearly three decades. In 1990, Woolley made a serendipitous finding that estrogen regulates the density of dendritic spines in the hippocampus of rat brains.
Nestled deep within the brain behind the ears, the hippocampus serves as the cognitive hub, boasting both gray and white matter and densely packed with sex hormone receptors. Remarkably responsive to change in volume, the hippocampus stands out as the brain region most receptive to adaptation. Activities like acquiring new skills, such as learning to juggle later in life or mastering maps for a London taxicab driving license exam, have been shown to expand the hippocampus. Conversely, a shrinking hippocampus can signify early signs of dementia, particularly in conditions like Alzheimer’s disease.
Following Woolley’s groundbreaking revelation, researchers have uncovered that menopause leads to a decrease in gray matter volume in certain brain regions. Yet, investigations have primarily provided a snapshot of volunteers’ brains at a singular time point. Scientists were keen to delve deeper, probing whether adult human brains undergo alterations during the monthly ebb and flow of sex hormones.
“Can we achieve utmost precision? Can we meticulously measure an individual’s brain 30, 50, or even 100 times?” pondered Jacobs. This curiosity spurred one scientist within Jacobs’ cohort to undergo daily brain scans for an entire month in 2020, seeking to unravel the mysteries of hormonal fluctuations on brain structure.
“She was akin to the Marie Curie of neuroscience,” remarks Jacobs. Through the 30 scans of this individual’s brain, Jacobs’ team uncovered how sex hormones sculpted the hippocampus and reconfigured brain connections. Yet, the swiftness with which hormonal fluctuations during the menstrual cycle induced these changes remained unclear.
In pursuit of answers, researchers in Leipzig and Santa Barbara have undertaken independent studies, scanning the brains of over 50 women at various points throughout their menstrual cycles. These efforts aim to shed light on the dynamics of hormonal influences on brain structure and function.
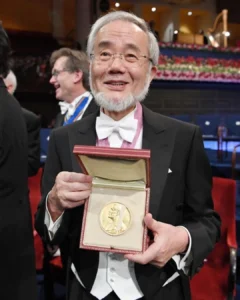
In a study published in the journal Nature Mental Health, Sacher’s team employed ultrasound to pinpoint the exact time of ovulation for 27 female volunteers. This enabled them to gather blood samples at six specific junctures during the menstrual cycle, aligned with ovulation and corresponding hormone levels. Subsequently, the researchers conducted ultrahigh-field MRI scans of the brains of these 27 women at six distinct time intervals.
Utilizing a more advanced MRI technology than typically used in clinical settings, Sacher’s team captured images of the live brain with unprecedented resolution, surpassing what was previously achievable without postmortem brain slicing.
Despite its diminutive size, the Sacher team discerned a meticulously orchestrated sequence of alterations within various regions of the hippocampus as it underwent remodeling synchronized with the menstrual cycle. The outer layer of the hippocampus thickened, while gray matter expanded in tandem with increasing estrogen levels and declining progesterone. However, with the ascent of progesterone levels, the memory-involved layer expanded.
In additional research, which has yet to undergo peer review, the brains of 30 volunteers were scanned during ovulation, menstruation, and the interim period between the two. This study revealed that not only did the thickness of gray matter fluctuate in response to hormonal cues, but also the structural characteristics of white matter.
“We essentially applied a measuring tool to gray matter and observed its synchronized changes alongside hormone fluctuations,” explains Elizabeth Rizor, who co-led the study alongside Viktoriya Babenko, both neuroscientists at the University of California Santa Barbara.
The findings suggest that hormonal fluctuations preceding ovulation could instigate alterations in white matter, potentially enhancing the efficiency of information transmission across various brain regions.
“These changes extend widely, affecting not only gray matter but also the regions responsible for coordinating interactions across brain areas and the white matter pathways,” remarks Babenko.
Nevertheless, the alterations detected in brain region volume or thickness in these studies have yet to be linked to specific cognitive functions. While the research demonstrates that certain brain areas can adapt in sync with hormonal fluctuations during the menstrual cycle, scientists urge caution in interpreting these findings as indicative of effects on memory or cognition.
“We cannot definitively conclude that larger size equates to enhanced performance in specific brain functions or processes,” emphasizes Woolley.
The studies also do not elucidate whether the observed volume changes are linked to the array of emotional and cognitive symptoms women encounter during their menstrual cycle. Interestingly, these studies specifically recruited healthy women who did not report experiencing any of these symptoms.
What these findings underscore is the pressing need for further research into understanding the distinct neurological requirements of women, remarks Jacobs.
“Real structural alterations are occurring in our brains that could potentially correlate with the fluctuations, the mood swings, or whatever symptoms women experience,” reflects Jashim.
Despite women representing 70 percent of Alzheimer’s disease cases and 65 percent of depression cases, only a minuscule fraction—around half of one percent—of brain imaging research pertains to women. This inequality persists even in drug approvals, exemplified by the recent approval of lecanemabirmb by the U.S. Food and Drug Administration for early Alzheimer’s disease treatment, despite potential ineffectiveness in slowing the disease progression in women.
“It’s long overdue to prioritize the brain as a central aspect of women’s health,” asserts Sacher.
Source: National Geographic, written by Sanjay Mishra, adapted by Stylisphere
stylisphere
most read